Connect With Us
Blog
Items filtered by date: April 2025
Athlete’s Foot and Its Causes

Athlete's foot, also known as tinea pedis, is a common fungal infection that affects the skin of the feet. It thrives in warm, moist environments such as locker rooms, public showers, and sweaty shoes. This condition often begins between the toes but can spread to other parts of the foot. Common symptoms include itching, burning, and stinging sensations, along with peeling or cracking skin. Redness and scaling may also appear, sometimes accompanied by an unpleasant odor. The fungus responsible for athlete's foot is contagious and can be contracted by walking barefoot on contaminated surfaces or sharing personal items. People who wear tight footwear or keep their feet damp for long periods are more at risk. Athlete’s foot can be uncomfortable and irritating. If you have developed this foot condition, it is suggested that you consult a podiatrist who can effectively treat athlete’s foot, which may include prescribed medication.
Athlete’s Foot
Athlete’s foot is often an uncomfortable condition to experience. Thankfully, podiatrists specialize in treating athlete’s foot and offer the best treatment options. If you have any questions about athlete’s foot, consult with Michael Schwartzman, DPM from Illinois and Indiana . Our doctor will assess your condition and provide you with quality treatment.
What Is Athlete’s Foot?
Tinea pedis, more commonly known as athlete’s foot, is a non-serious and common fungal infection of the foot. Athlete’s foot is contagious and can be contracted by touching someone who has it or infected surfaces. The most common places contaminated by it are public showers, locker rooms, and swimming pools. Once contracted, it grows on feet that are left inside moist, dark, and warm shoes and socks.
Prevention
The most effective ways to prevent athlete’s foot include:
- Thoroughly washing and drying feet
- Avoid going barefoot in locker rooms and public showers
- Using shower shoes in public showers
- Wearing socks that allow the feet to breathe
- Changing socks and shoes frequently if you sweat a lot
Symptoms
Athlete’s foot initially occurs as a rash between the toes. However, if left undiagnosed, it can spread to the sides and bottom of the feet, toenails, and if touched by hand, the hands themselves. Symptoms include:
- Redness
- Burning
- Itching
- Scaly and peeling skin
Diagnosis and Treatment
Diagnosis is quick and easy. Skin samples will be taken and either viewed under a microscope or sent to a lab for testing. Sometimes, a podiatrist can diagnose it based on simply looking at it. Once confirmed, treatment options include oral and topical antifungal medications.
If you have any questions, please feel free to contact our offices located in West Chicago, IL and Whiting, IN . We offer the newest diagnostic and treatment technologies for all your foot care needs.
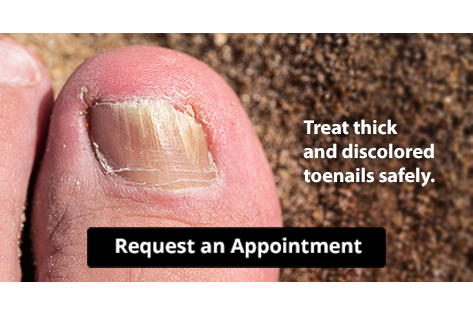
Stop Your Toenail Fungus
Plantar Fasciitis Pain and Its Impact on Walking

Plantar fasciitis involves inflammation of the thick band of tissue that runs along the bottom of the foot, connecting the heel to the toes. This tissue, called the plantar fascia, supports the arch and absorbs shock during movement. When it becomes irritated or strained, sharp heel pain can develop, especially during the first steps in the morning or after long periods of rest. This discomfort can make walking difficult and alter the natural gait, leading to further strain on the feet and legs. Factors that can worsen plantar fasciitis include standing for extended periods, wearing shoes with inadequate support, having flat feet or high arches, and engaging in repetitive activities. If you have heel pain, it is suggested that you promptly contact a podiatrist who can offer appropriate treatment solutions.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Michael Schwartzman, DPM from Illinois and Indiana . Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our offices located in West Chicago, IL and Whiting, IN . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Exploring Offloading Aids for Foot Ulcers

Offloading devices are used to reduce pressure on specific areas of the foot where ulcers have formed, helping to prevent further damage and support healing. Offloading devices typically shift body weight away from the wound, which decreases friction and mechanical stress. Total contact casts provide the highest level of pressure relief by fully immobilizing the foot and ankle, making them effective for deep or persistent ulcers. For patients needing more flexibility, removable cast walkers not only offer protection but also allow access for wound inspection. Custom orthotics and specialized shoes with cushioned soles are often used for less severe ulcers or during the later stages of healing. Offloading sandals and pneumatic boots may help with minor ulcers by offering light support and comfort for indoor use. Choosing the right device depends on the size and depth of the ulcer, the location on the foot, and the patient’s ability to move independently. If you have foot ulcers that require wound care, it is suggested that you schedule an appointment with a podiatrist to see if offloading devices may work for you.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Michael Schwartzman, DPM from Illinois and Indiana . Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our offices located in West Chicago, IL and Whiting, IN . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Causes of Arch Pain

Arch pain can affect people of all activity levels. The arch of the foot supports body weight, absorbs impact, and helps stabilize movement. Pain in this area may be linked to plantar fasciitis, the most common cause, where the ligament connecting the heel to the toes becomes inflamed from overuse or strain. Another cause of arch pain is posterior tibial tendon dysfunction, which occurs when the tendon that supports the arch weakens or becomes injured. Cavus foot, a condition involving unusually high arches, may lead to instability and pressure-related discomfort. Overpronation, where the foot rolls inward excessively while walking, can also place undue stress on the arch and nearby joints. Risk factors such as weight gain, aging, and repetitive stress on the feet may contribute to these conditions. Arch pain is sometimes felt in the heel, ball of the foot, or ankle, and may worsen during or after standing or walking. If you have pain in the arch of your foot, it is suggested that you schedule an appointment with a podiatrist for an exam and appropriate treatment.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with Michael Schwartzman, DPM from Illinois and Indiana . Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our offices located in West Chicago, IL and Whiting, IN . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Preventing Toenail Fungus

Toenail fungus, or onychomycosis, is a fungal infection that causes toenails to become discolored, thickened, brittle, or even separated from the nail bed. The infection often starts as a white or yellow spot under the tip of the nail, gradually spreading deeper. Symptoms may include a foul odor, pain, or discomfort while wearing shoes. Toenail fungus is typically caused by exposure to warm, moist environments, such as communal showers, around swimming pools, or tight, non-breathable shoes. People with a weakened immune system, diabetes, or poor circulation are more at risk of developing this condition. To prevent toenail fungus, it is essential to practice good foot hygiene by keeping your feet dry, wearing moisture-wicking socks, and choosing breathable shoes. Avoid walking barefoot in public spaces and regularly trim your nails straight across. A podiatrist can treat toenail fungus with antifungal medications or nail removal in severe cases. If you have the beginning symptoms of toenail fungus, it is suggested that you schedule an appointment with a podiatrist.
If left untreated, toenail fungus may spread to other toenails, skin, or even fingernails. If you suspect you have toenail fungus it is important to seek treatment right away. For more information about treatment, contact Michael Schwartzman, DPM of Illinois and Indiana . Our doctor can provide the care you need to keep you pain-free and on your feet.
Symptoms
- Warped or oddly shaped nails
- Yellowish nails
- Loose/separated nail
- Buildup of bits and pieces of nail fragments under the nail
- Brittle, broken, thickened nail
Treatment
If self-care strategies and over-the-counter medications does not help your fungus, your podiatrist may give you a prescription drug instead. Even if you find relief from your toenail fungus symptoms, you may experience a repeat infection in the future.
Prevention
In order to prevent getting toenail fungus in the future, you should always make sure to wash your feet with soap and water. After washing, it is important to dry your feet thoroughly especially in between the toes. When trimming your toenails, be sure to trim straight across instead of in a rounded shape. It is crucial not to cover up discolored nails with nail polish because that will prevent your nail from being able to “breathe”.
In some cases, surgical procedure may be needed to remove the toenail fungus. Consult with your podiatrist about the best treatment options for your case of toenail fungus.
If you have any questions, please feel free to contact our offices located in West Chicago, IL and Whiting, IN . We offer the newest diagnostic and treatment technologies for all your foot care needs.